Composite Blood Vessel Substitute and ahe Method for Producing it
The result was created within the framework of many years of cooperation of an interdisciplinary scientific research team including experts from the ranks of physicians (General University Hospital in Prague, 1st Faculty of Medicine, Charles University in Prague), technicians, material and process engineers (Faculty of Mechanical Engineering, Czech Technical University in Prague). The cooperation was primarily carried out within the project obtained from the Ministry of Health NT13302-4/2012, NV15-27941A. Since 2025, further replacement optimization has been underway within the framework of another follow-up project. This is a composite vascular graft (prosthesis) with a sandwich wall structure based on a combination of biological and synthetic polymers. The prosthesis is primarily designed for topographic anatomical areas with low blood flow (below 200 ml/min) and small clearances (below 6 mm). This type of prosthesis has not yet been satisfactorily addressed, yet due to modern dynamic times and lifestyles, there is a significant worldwide increase in cardiovascular disease. In the international context, for example, the Czech Republic is ranked among the countries with a high cardiovascular risk. In recent years, cardiovascular disease has accounted for up to 42% of all mortality in the population.
The work on the design of the vascular graft has been granted Czech patent CZ308556 and European patent EP3434292.
The result is relevant to the healthcare and prosthetics industry. In vascular surgery, the vena saphena magna (VSM) or vena saphena parva (VSP) is the gold standard when creating a bypass or fully replacing an affected vascular segment. These are autologous vascular grafts from the lower limb. This method of reconstruction is often not possible due to unavailable or poor-quality vascular grafts, e.g., due to vascular disease. For example, varicose veins affect these veins. This disease occurs in up to 30 % of women and 20 % of men. Therefore, synthetic vascular grafts, knitted, woven, or cast, are often used. However, they have several limitations. The most important ones are low resistance to infection, increased risk of closure or stenosis, or, on the contrary, dilatation over time due to environmental and body conditions. In some prostheses, a bovine collagen plug is applied, to which up to 3 % of the population has an increased allergic reaction.
Our alternative vascular prosthesis consists of a matrix of fish collagen into which is integrated a scaffold of knitted fabric consisting of monofilament polymer fibers. The matrix of freshwater fish-derived collagen is produced by extrusion technology, which involves the orientation (arrangement) of the collagen fiber bundles. This type of technology, together with the geometry of the scaffold, creates anisotropy in the wall material of the artificial substitute, even though the original raw material is isotropic. This brings the internal structure and mechanical response closer to that of the native vessel.
A great advantage is therefore the minimization of allergic reaction of the recipient's organism and good healing in the area of anastomoses. The elimination of the risk of transmission of zoonoses known to occur in warm-blooded animals is essential. Preclinical tests have been carried out on large animals (sheep) with the new substitute. Low immunogenicity, very good healing in the anastomosis area, rapid colonization of the inner surface by endothelial cells (neointima formation), and a reduced risk of prosthesis occlusions at low blood flow have been demonstrated.
The application is expected in the area of coronary and low-diameter vessels and bypasses and the periphery, especially pedal replacements and bypasses, e.g., when maintaining or restoring blood supply to the limb due to diabetes. Up to 10% of the population in the Czech Republic is affected by diabetes. Worldwide, where the disease is registered, there are approximately 540 million people with diabetes. The annual worldwide estimate of deaths from this disease (and complications arising from it) is around 7 million people. Vascular replacements of various types have a major impact on maintaining or restoring an individual's quality of life. In many cases, it is a life-saving intervention, an application. Anatomically and functionally, the alternative artificial vascular graft may be applicable in the entire population, i.e. women, men, and possibly children.
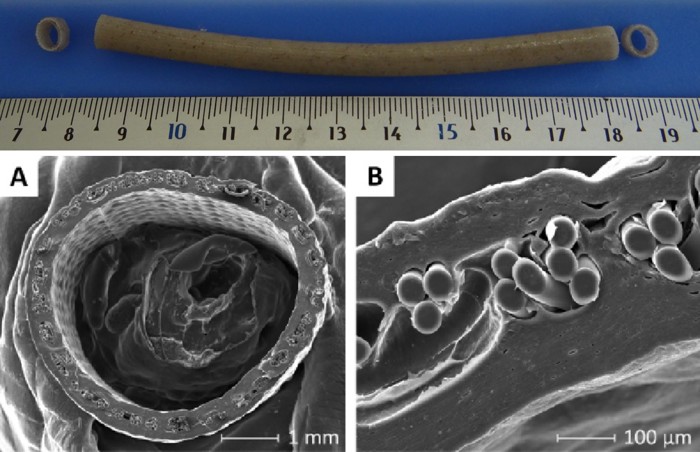
Fig. 1 Composite vascular replacement for small diameters and low flow rates with a sandwich wall construction. A-B cross-section through the wall of the artificial vascular graft.
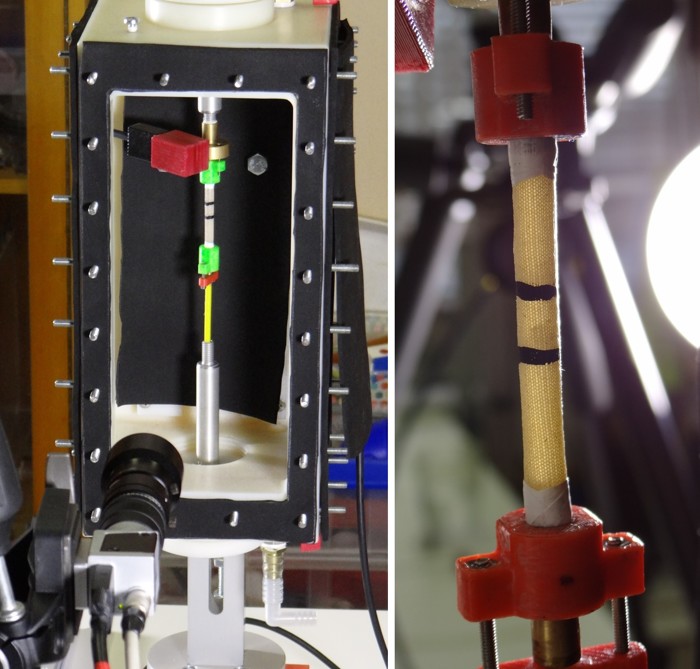
Fig. 2 Mechanical tests of artificial vascular replacement in the system for inflation-extension tests at the Faculty of Mechanical Engineering, CTU in Prague, i.e., cyclic loading of a tubular specimen by internal fluid pressure.
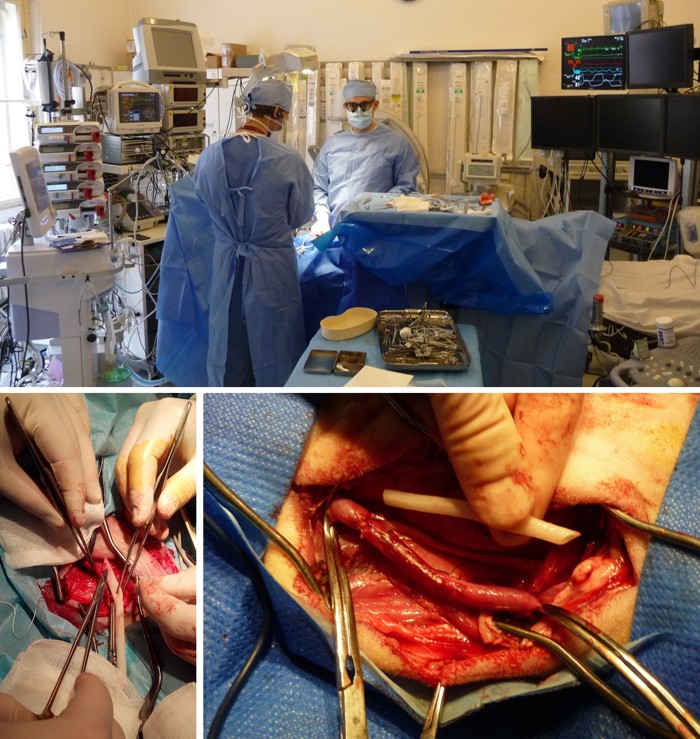
Fig. 3 Implantation of a prototype vascular graft into an animal model, i.e., the carotid artery of a sheep, by anastomosis End-to-Side or End-to-End. Experimental operating room at the 1st Faculty of Medicine, Charles University in Prague, and cardiac surgeons from the General University Hospital in Prague.

Fig. 4 Measurement of internal dimensions of implanted vascular graft by ultrasound, transverse and longitudinal cross-section.
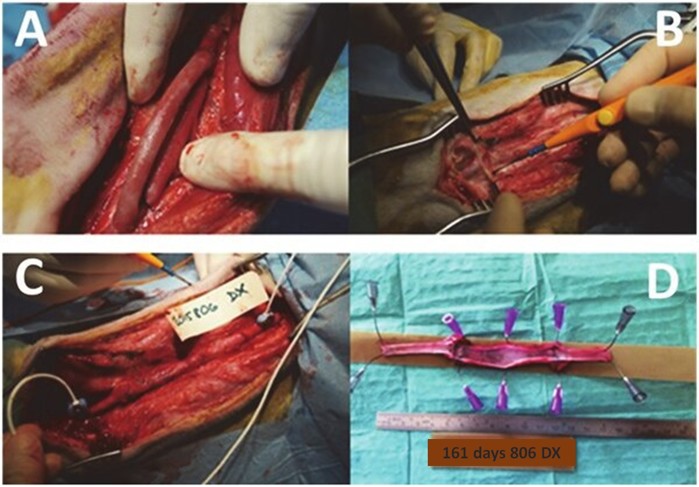
Fig. 5 Implanted a prosthesis in the carotid artery and explanted the graft after 161 days.
A: proximal and distal anastomosis End-to-Side, ligation of the carotid artery; B: explantation of patent graft; C: flow
measurement with ultrasound probes; D: no macroscopic signs of intimal hyperplasia after 161 days.
- EP3434292A1 - COMPOSITE BLOOD VESSEL SUBSTITUTE AND THE METHOD FOR PRODUCING IT
- CZ308556B6 Composite vascular replacement and manufacturing method
Contact:
Ing. Hynek Chlup, Ph.D.
Department of Mechanics, Biomechanics and Mechatronics FME CTU in Prague
E-mail: hynek.chlup@cvut.cz
Phone: +420 224 352 690
![[design/2014/cvut-logo-en-white.png]](https://fs.cvut.cz/content/images/design/2014/cvut-logo-en-white.png)
![[design/2014/cvut-logo-en-print.jpg]](https://fs.cvut.cz/content/images/design/2014/cvut-logo-en-print.jpg)